How to Manage Withdrawal Symptoms: A Doctor-Approved Safety Guide
Aug 14, 2025
Recent surveys reveal a startling fact - more than 11% of Americans aged 12 and older used illicit substances in just one month . Many people who try to stop substance use face dangerous withdrawal symptoms.
Alcohol withdrawal impacts about 50% of people with alcohol use disorder who stop or substantially decrease their alcohol consumption . The duration of withdrawal varies by substance. Medication withdrawal symptoms can last anywhere from a few days to several weeks . Some drug withdrawal symptoms cause mild discomfort, while others can become life-threatening without proper medical care .
The process brings numerous challenges that need careful attention. Conditions like delirium tremens can turn fatal in about 15% of alcohol withdrawal cases without proper care . The dangers increase especially when you have prescription medications that are stopped suddenly. This sudden stop can trigger severe medication withdrawal symptoms and even Post Acute Withdrawal Syndrome (PAWS) .
This complete guide offers doctor-approved strategies to help you manage withdrawal symptoms safely. You'll learn to recognize warning signs and find appropriate support through this challenging journey.
Understanding Withdrawal: What Happens in the Body
Your body works through a delicate balance of chemical processes. Substances can disrupt this balance, and your body works hard to restore equilibrium—a process called homeostasis. This amazing adaptation system creates the mechanism behind withdrawal symptoms.
What causes withdrawal symptoms?
Your body responds to substance reduction or cessation after long-term use through withdrawal syndromes [1]. Withdrawal symptoms appear as your body tries to reach a new state of homeostasis while clearing out any remaining chemical influence [2].
Your body's compensatory physiological adaptation to continuous substance exposure creates withdrawal symptoms [1]. These adaptations vary with different substances, which creates unique withdrawal patterns based on what you've taken.
Bodies develop counter-regulatory mechanisms to maintain balance during substance exposure. These mechanisms produce unopposed effects when you suddenly remove the substance, which triggers withdrawal symptoms [3]. This explains why stopping certain substances "cold turkey" becomes uncomfortable and potentially dangerous.
How dependence guides withdrawal
Physical dependence happens when stopping a substance creates a specific withdrawal syndrome [1]. Your body adapts to work with the substance present, which causes this dependence.
Substances might bring pleasure or relief at first, but your brain adjusts to their presence with continued use [2]. You might need bigger doses to get the same effect—this is tolerance [1]. The substance becomes necessary just to feel normal [1].
Tolerance grows through dose, duration, and frequency of use. This results from metabolic adaptation or cellular/functional changes [3]. These adaptations create withdrawal symptoms that range from mild discomfort to severe, life-threatening conditions when substance levels drop.
Physical dependence demonstrates differently from addiction, though they often occur together. It's worth mentioning that people using medications as prescribed can develop physical dependence after just two weeks of regular use [2].
The role of brain chemistry in withdrawal
Complex changes in neurotransmitter systems create the neurochemical basis of withdrawal. Brain chemistry changes during substance use create imbalances that show up during withdrawal.
For example:
-
Alcohol and benzodiazepines affect GABA (inhibitory) and glutamate (excitatory) systems. Long-term use decreases GABA receptors and increases glutamate receptors, which creates an excitatory state during withdrawal [3].
-
Opioids control pain through hyperpolarization and neuron inhibition. Regular use reduces this effectiveness and increases excitatory pathways [1].
-
Stimulants boost dopamine and other neurotransmitter levels. Decreased dopamine activity creates negative emotional states during withdrawal [4].
These brain chemistry changes explain why withdrawal includes both physical and psychological symptoms. The withdrawal/negative affect stage follows the binge/intoxication stage and creates future rounds of substance use [4]. Taking substances to relieve withdrawal makes symptoms worse the next time you stop—creating a vicious cycle [4].
Brain imaging studies show lasting decreases in dopamine D2 receptors in addicted individuals [4]. Stress neurotransmitters like corticotropin-releasing factor, norepinephrine, and dynorphin activate during withdrawal and contribute to negative emotions [4].
Understanding these complex brain mechanisms shows why proper medical support helps manage withdrawal safely.
Common Drug and Medication Withdrawal Symptoms
Withdrawal symptoms look different for each substance. They range from mild discomfort to conditions that could threaten your life. People who recognize these symptoms can better prepare and manage their withdrawal safely.
Physical symptoms to expect
The body reacts to withdrawal much like a severe illness, causing pain everywhere. Your age, overall health, the type of substance, and how long you used it determine how intense these symptoms become [5].
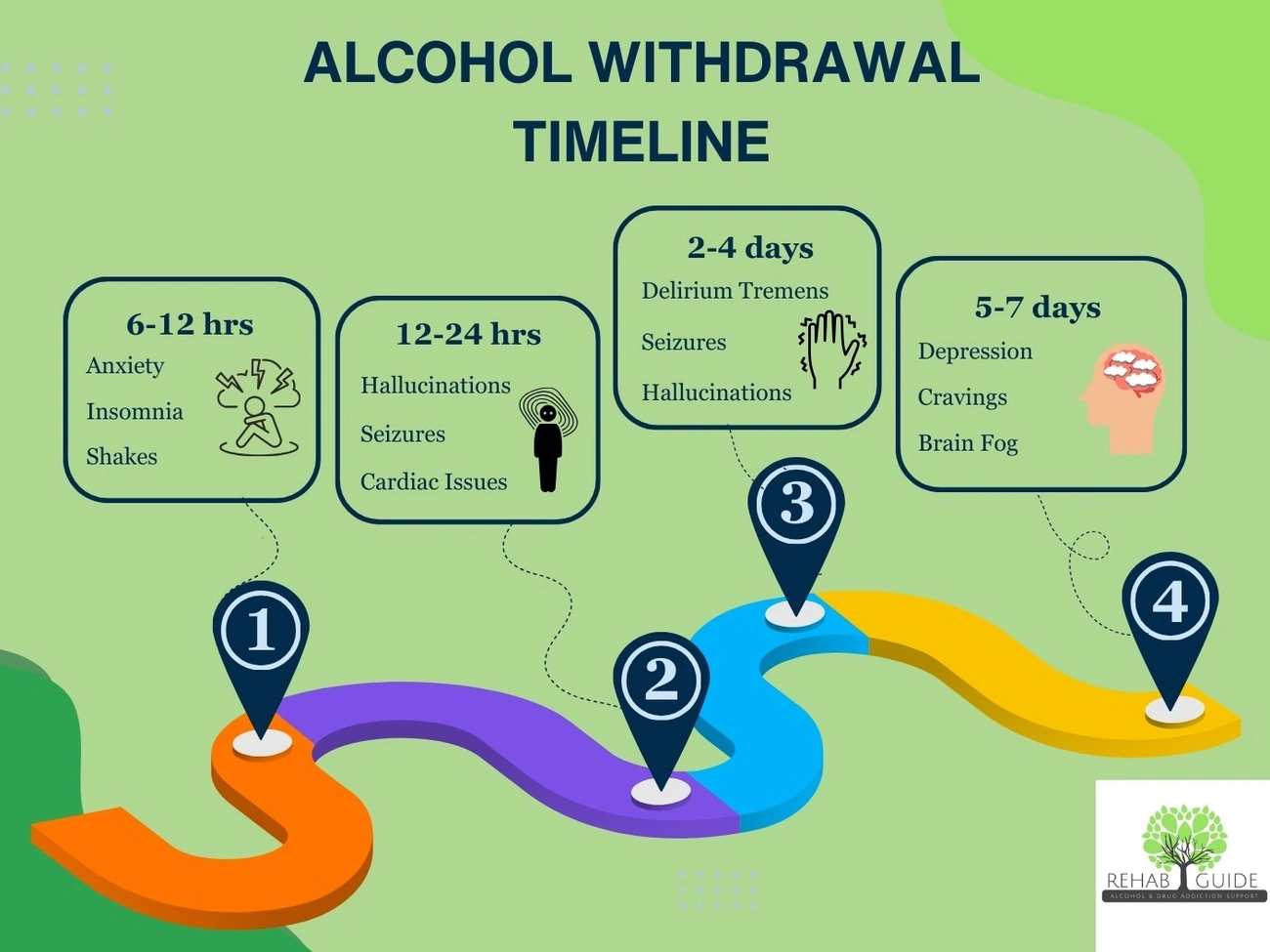
When you stop drinking alcohol, physical symptoms usually show up within 6-24 hours and get worse between 36-72 hours [4]. You might experience:
-
Heavy sweating and shaking hands
-
Racing heart and high blood pressure
-
Nausea, vomiting, and diarrhea
-
Dehydration and sleep problems [4]
Opioid withdrawal feels like a terrible case of flu. While it rarely threatens your life, it can be extremely painful [6]. Your body demonstrates symptoms like muscle and joint pain, bigger pupils, constant yawning, runny nose, hot and cold flashes, and stomach problems [4][1].
Benzodiazepine withdrawal looks a lot like alcohol withdrawal because both affect GABA receptors similarly [2]. The body responds with tight muscles, aches, shaking, and sometimes dangerous seizures [6].
Stimulant withdrawal works differently. You'll mostly sleep more, eat more, and feel muscle aches and extreme tiredness. Some people also shake [4][1].
Emotional and psychological effects
The mind struggles just as much as the body during withdrawal, and these mental challenges often last longer [7]. Physical symptoms follow patterns we can predict, but psychological effects can pop up randomly. They might return during stressful times, even months after you've stopped using [7].
The mind reacts to withdrawal in several ways:
Almost everyone feels anxious and irritable when their brain chemistry changes during withdrawal [8]. People who quit stimulants often feel depressed and can't enjoy things because their dopamine levels drop [9]. Alcohol and benzodiazepine withdrawal can mess with your thinking, making it hard to focus, remember things, or think clearly [9]. Cravings might be the toughest mental challenge, pushing people to use again even when they know it's harmful [8].
Studies show that your mental state plays a vital role in how bad withdrawal gets. Research proves that anxiety, depression, and pain make withdrawal symptoms much worse [10].
Symptoms of medication withdrawal vs. drug withdrawal
Prescription and street drug withdrawal share many symptoms, but they're different in important ways.
When you stop taking prescribed benzos or pain pills, your original health problems might come back stronger [11]. This makes it tough to tell if you're dealing with withdrawal or your old symptoms.
Prescription withdrawal usually follows a clearer path because doctors know exactly what's in your medication [2]. Notwithstanding that, stopping antidepressants suddenly can cause antidepressant discontinuation syndrome. You might feel dizzy, get headaches, or experience "brain zaps" [12].
Street drugs create extra problems because you never know what's really in them or how strong they are [1]. Your mind suffers more than your body when you quit stimulants like cocaine and meth [1].
Both types of withdrawal need medical supervision. Having doctors watch over you makes withdrawal safer and increases your chances of staying clean.
How Long Does Withdrawal Last?
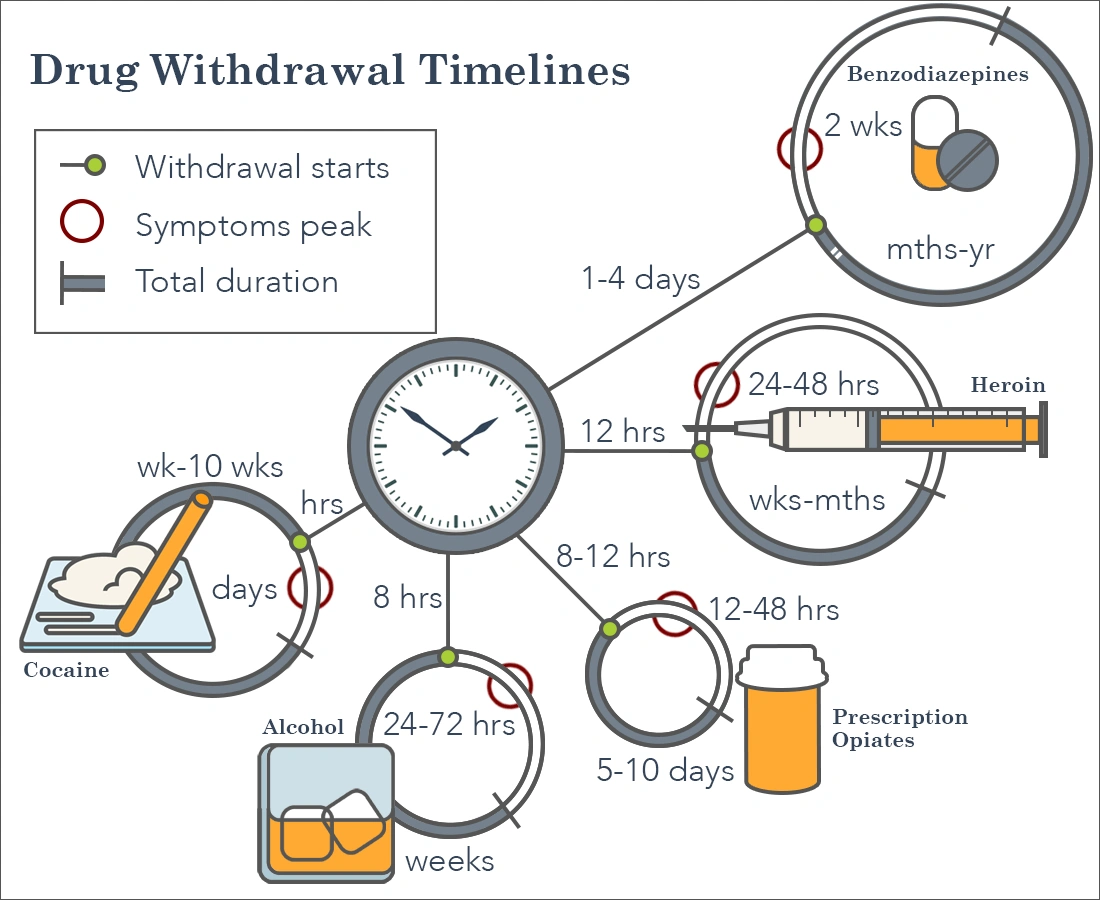
The time it takes to withdraw from substances can vary significantly. Knowing these timeframes helps people prepare both mentally and physically for what lies ahead.
Short-acting vs. long-acting substances
A substance's half-life determines when withdrawal starts and its duration. Short-acting substances quickly exit the body and trigger more intense withdrawal symptoms earlier. Long-acting substances stay in the system longer, which delays the onset but might stretch out the overall withdrawal period.
To name just one example, people taking short-acting benzodiazepines like Xanax or Ativan usually experience withdrawal symptoms 1-2 days after their last dose. Long-acting benzodiazepines such as Valium might not show withdrawal effects until 2-7 days after stopping [13][14].
Typical timelines for alcohol, opioids, and benzos
Alcohol withdrawal starts 6-24 hours after the last drink. Symptoms peak between 24-72 hours and usually clear up within 5-10 days [4][15]. Some people might experience symptoms like insomnia and mood changes that last weeks or months [15].
Opioid withdrawal differs based on the specific drug:
-
Short-acting opioids (heroin, immediate-release formulations): Symptoms start within 8-24 hours, peak at 36-72 hours, and last 4-10 days [4][16][17].
-
Long-acting opioids (methadone, extended-release formulations): Withdrawal might not begin until 12-48 hours after the last dose and can stretch for 10-20 days [4][17].
Benzodiazepine withdrawal takes longer. Symptoms appear within 1-4 days and peak during the first two weeks. The acute phase might last several weeks [18]. About 10% of people experience symptoms that persist for years after stopping [13].
Factors that affect withdrawal duration
Many elements determine how long withdrawal symptoms last:
-
Substance specifics (type, potency, half-life)
-
Duration and frequency of use
-
Typical dosage amount
-
Individual factors (age, metabolism, overall health)
-
Underlying medical or mental health conditions
-
Multiple substance use
-
Previous withdrawal experiences
The way someone takes substances affects withdrawal timing. Injecting or snorting substances usually brings on withdrawal symptoms faster than taking them orally [13].
These timelines help set realistic expectations, but each person's experience remains unique. The mix of substance characteristics and personal factors creates an individual withdrawal pattern for everyone.
Safe Ways to Manage Withdrawal Symptoms
Medical support and personal care strategies work together to manage withdrawal safely. Professional supervision, proper medications, and self-care techniques build the strongest foundation for recovery.
When to seek medical detox
Medical detoxification becomes vital in several situations. Alcohol withdrawal can threaten your life when severe, which makes medical detox a must rather than a choice [3]. Benzodiazepine withdrawal can cause dangerous seizures that could be deadly without medical help [3].
Medical detox proves necessary for people who show physical and psychological signs of substance dependence [3]. Professional supervision becomes vital if you've had severe withdrawal symptoms before or have existing medical conditions [21]. People who drink heavily, have a history of withdrawal seizures, or are over 65 should get medical care [22].
Medications used during withdrawal
Several medications help manage withdrawal symptoms:
-
For alcohol withdrawal: Benzodiazepines (chlordiazepoxide, diazepam, lorazepam) are the primary treatment to reduce seizure risk [15]. Beta-blockers or clonidine can help with high blood pressure and rapid heart rate if symptoms persist [15].
-
For opioid withdrawal: Methadone (used since the 1950s), buprenorphine products like Suboxone, and naltrexone help control cravings and symptoms [3]. Lofexidine targets specific withdrawal symptoms [23].
-
For multiple substances: Some medications target specific symptoms - acetaminophen helps with muscle aches [3] while anticonvulsants prevent seizures [24].
Hydration, nutrition, and rest
Your body needs 2-3 liters of water daily to replace fluids lost through sweating and diarrhea [4]. Dehydration makes withdrawal more uncomfortable and risky [5].
A balanced diet rich in fruits, vegetables, lean proteins, and complex carbohydrates helps your recovery [25]. This diet puts back nutrients that substance use depleted [25] and gives you energy to heal.
Sleep plays a key role - it regulates mood, lowers blood pressure, and lets cells repair themselves [26]. Set regular sleep hours and take naps when your body needs them.
Mind-body techniques for relief
Mind-body approaches are a great way to get extra support. Studies show mindfulness-based methods cut cravings by up to 20% and reduce relapse rates by 30% [27]. These techniques help you handle uncomfortable feelings without using substances.
Three approaches that work well:
-
Mindfulness-Based Relapse Prevention (MBRP): Helps you spot triggers before they lead to substance use [28]
-
Mindfulness-Oriented Recovery Enhancement (MORE): Uses mindfulness and positive psychology to deal with underlying stress [28]
-
"Urge surfing": Shows you how to observe emotions and sensations without acting on them [28]
Note that withdrawal management alone rarely leads to long-term sobriety—it's a vital first step before starting psychological treatment [4].
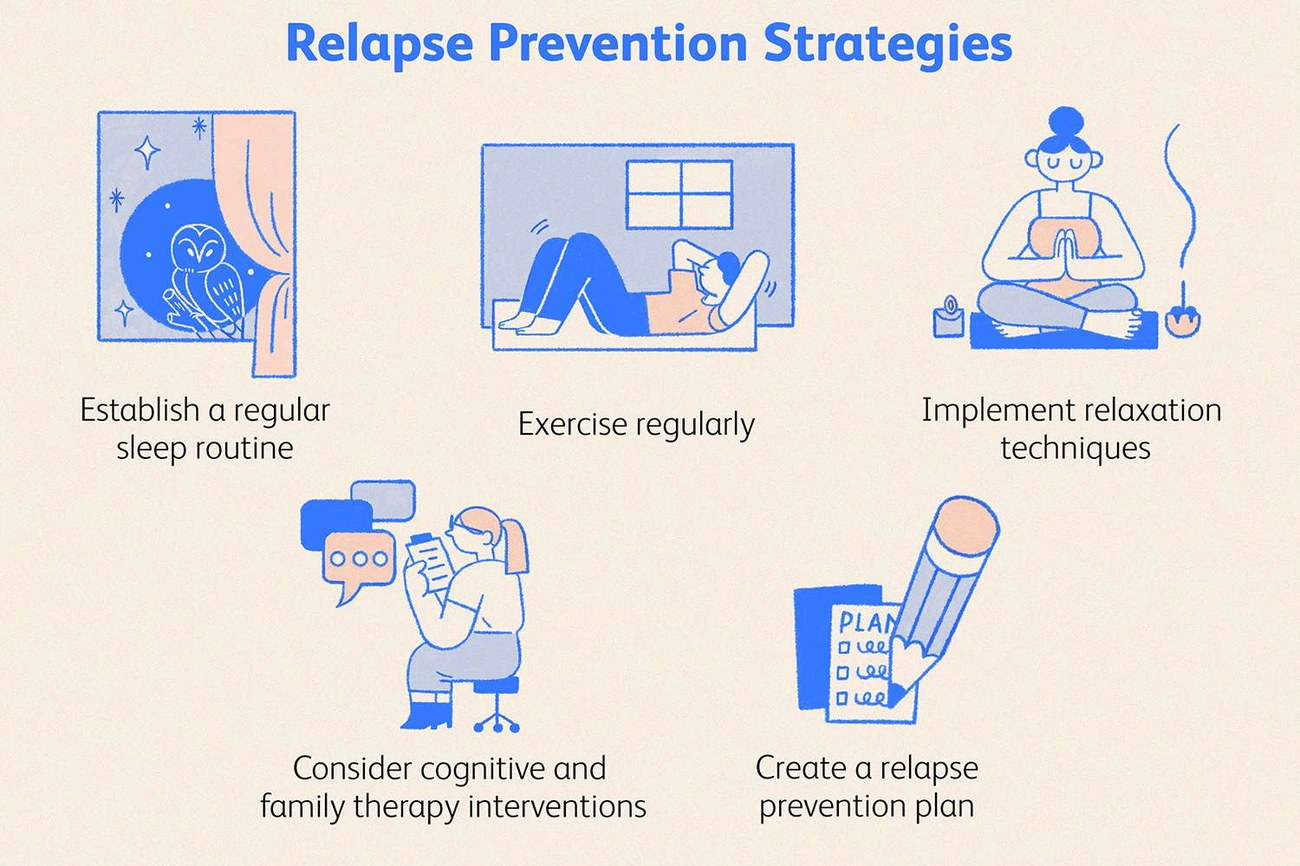
Preventing Complications and Relapse
Staying alert remains significant even after acute withdrawal symptoms go away. In fact, spotting warning signs early can prevent life-threatening complications.
Recognizing warning signs of severe withdrawal
Severe withdrawal just needs immediate medical attention. Watch for delirium tremens in alcohol withdrawal. This condition shows up as agitation, fever, hallucinations, and severe confusion—and can be fatal in 5-10% of cases [15]. Other critical warning signs include seizures, irregular heartbeat, or high fever [29]. Symptoms can worsen unexpectedly, whatever they look like at first [15].
Post-acute withdrawal syndrome (PAWS)
About 75% of recovering individuals face Post-Acute Withdrawal Syndrome (PAWS) after acute withdrawal ends [30]. This condition shows up as negative emotions during early abstinence and can last 4-6 months or longer [30]. People experience anxiety, depression, cognitive problems, sleep issues, irritability, and powerful cravings [31].
PAWS symptoms come and go like waves—here one day, gone the next—and slowly decrease in both intensity and frequency [32]. These symptoms remain most important relapse risk factors throughout recovery [30].
Building a support system
Research shows that people with access to peer-based support use fewer substances and relapse less often [33]. Strong support networks include:
-
Professional resources (counselors, therapists, doctors)
-
Recovery peers (12-step programs, recovery groups)
-
Supportive family and friends
-
Sponsors who provide mentorship and accountability
People often relapse when they feel isolated, depressed, anxious, or bored [34].
Transitioning to long-term treatment
Recovery goes beyond detoxification. Relapse rates reach about 50% within 12 weeks without follow-up treatment [35]. These transition strategies work well:
-
Medication options like naltrexone or acamprosate can reduce relapse rates by up to 25% [8]
-
Continued therapy that focuses on relapse prevention skills
-
Structured aftercare programs that offer ongoing support
-
Daily routines that limit trigger exposure [7]
Note that detoxification alone rarely creates lasting recovery. The shift to detailed treatment builds the foundation for permanent change.
Conclusion
Getting clean from substances is tough but needed to recover. This piece shows how our bodies react when substances leave our system. The complex neurochemical processes behind withdrawal symptoms affect everyone differently. Understanding why this happens gives you better insight into what you might face during this tough time.
Withdrawal symptoms can vary substantially based on what substance you used. Some people might feel mild discomfort for a few days. Others could face intense physical and psychological symptoms for weeks. Medical supervision becomes vital, especially when you have alcohol and benzodiazepine withdrawal that could threaten your life.
On top of that, combining medical support with personal care offers the safest path forward. Medical detox gives you vital monitoring and medication to reduce symptoms. Your body heals better with proper hydration, nutrition, and rest. Mind-body techniques help you handle cravings and emotional stress better.
The first phase of withdrawal marks just the beginning of recovery. Many people experience Post-Acute Withdrawal Syndrome (PAWS) with symptoms that come in waves for months. You'll need a strong support system during this time. People who understand what you're going through can help guide you when things get tough.
Long-term recovery works best when you move from detox to detailed treatment. This helps you understand why it happens while teaching you skills to avoid relapse.
Withdrawal might look scary, but you can get through it safely with proper medical help, self-care, and ongoing treatment. Taking that first step to get help puts you on the path to better health and a life free from substances.
Key Takeaways
Managing withdrawal symptoms safely requires understanding the process, recognizing danger signs, and combining medical supervision with self-care strategies for the best outcomes.
• Seek medical detox for alcohol and benzodiazepine withdrawal - These can cause life-threatening seizures and delirium tremens requiring professional monitoring and medication management.
• Withdrawal duration varies by substance type - Short-acting drugs cause earlier, intense symptoms while long-acting substances delay onset but extend duration.
• Support acute withdrawal with hydration, nutrition, and rest - Drink 2-3 liters daily, eat balanced meals, and prioritize sleep to help your body heal.
• Build a strong support network early - Peer support reduces relapse risk by up to 30% through accountability, mentorship, and shared recovery experiences.
• Prepare for Post-Acute Withdrawal Syndrome (PAWS) - 75% experience fluctuating symptoms like anxiety and cravings for 4-6 months after acute withdrawal ends.
• Transition to comprehensive treatment after detox - Detoxification alone has 50% relapse rates within 12 weeks; ongoing therapy and medication improve long-term success.
Remember that withdrawal is just the first step in recovery. While the process can be challenging and potentially dangerous without proper care, combining medical supervision with personal wellness strategies and ongoing support creates the strongest foundation for lasting recovery and a healthier future.
FAQs
Q1. How long does drug withdrawal typically last? The duration of withdrawal varies depending on the substance, but it generally ranges from a few days to several weeks. Short-acting drugs like heroin may cause withdrawal symptoms for 4-10 days, while long-acting substances like methadone can lead to symptoms lasting 10-20 days.
Q2. What are some common withdrawal symptoms? Common withdrawal symptoms include anxiety, irritability, nausea, sweating, tremors, and insomnia. The specific symptoms and their intensity can vary based on the substance used, duration of use, and individual factors.
Q3. Is it safe to detox at home? Detoxing at home can be dangerous, especially for alcohol and benzodiazepine withdrawal, which can lead to life-threatening complications. It's always safest to undergo withdrawal under medical supervision to manage symptoms and prevent potential complications.
Q4. How can I manage withdrawal symptoms? Managing withdrawal symptoms involves a combination of medical support, proper hydration, nutrition, rest, and mind-body techniques. Medications may be prescribed to ease specific symptoms, while maintaining a balanced diet and getting adequate sleep can support the body's healing process.
Q5. What is Post-Acute Withdrawal Syndrome (PAWS)? Post-Acute Withdrawal Syndrome (PAWS) is a condition that affects about 75% of people in recovery. It involves predominantly emotional and psychological symptoms that can persist for 4-6 months or longer after acute withdrawal ends. Symptoms of PAWS include anxiety, depression, sleep disturbances, and intense cravings.
References
[1] - https://americanaddictioncenters.org/withdrawal-timelines-treatments
[2] - https://www.ncbi.nlm.nih.gov/books/NBK459239/
[3] - https://www.therecoveryvillage.com/treatment-program/medical-detox/
[4] - https://www.ncbi.nlm.nih.gov/books/NBK310652/
[5] - https://evokewellnessma.com/blog/nutrition-hydration-drug-alcohol-detox/
[6] - https://emedicine.medscape.com/article/819502-overview
[7] - https://www.therecoveryvillage.com/treatment-program/aftercare/how-to-stay-sober-after-rehab/
[8] - https://jamanetwork.com/journals/jamapsychiatry/fullarticle/207038
[9] - https://lagunatreatment.com/addiction-research/drug-withdrawal/psychological-withdrawal/
[10] - https://www.sciencedirect.com/science/article/pii/S0740547221001124
[11] - https://www.health.com/withdrawal-7967001
[12] - https://en.wikipedia.org/wiki/Drug_withdrawal
[13] - https://americanaddictioncenters.org/benzodiazepine/length-of-withdrawal
[14] - https://www.healthywa.wa.gov.au/Articles/A_E/Benzodiazepine-withdrawal
[15] - https://my.clevelandclinic.org/health/diseases/alcohol-withdrawal
[16] - https://www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/clinical+resources/clinical+programs+and+practice+guidelines/substance+misuse+and+dependence/substance+withdrawal+management/opioid+withdrawal+management
[17] - https://americanaddictioncenters.org/opioids/withdrawal-detox
[18] - https://www.highfocuscenters.com/2024/07/03/benzodiazepine-withdrawal-duration-timeline-and-symptoms/
[19] - https://adf.org.au/reducing-risk/withdrawal/
[20] - https://drughelpline.org/how-long-do-withdrawal-symptoms-last/
[21] - https://americanaddictioncenters.org/alcohol/withdrawal-detox
[22] - https://www.camh.ca/en/professionals/treating-conditions-and-disorders/alcohol-use/alcohol-use---treatment/treatment---treatment-for-alcohol-withdrawal
[23] - https://nida.nih.gov/research-topics/opioids/medications-opioid-overdose-withdrawal-addiction-infographic
[24] - https://oxfordtreatment.com/addiction-treatment/detox/common-medications/
[25] - https://evokewellnesstx.com/blog/nutrition-and-hydration-in-detox-supports-recovery/
[26] - https://diamondhousedetox.com/8-helpful-ways-to-cope-with-drug-withdrawal/
[27] - https://evokewellnessoh.com/blog/detox-and-mindfulness-during-withdrawal/
[28] - https://www.health.harvard.edu/blog/mind-body-medicine-in-addiction-recovery-2020102821239
[29] - https://medlineplus.gov/ency/article/000764.htm
[30] - https://pmc.ncbi.nlm.nih.gov/articles/PMC9798382/
[31] - https://www.hazeldenbettyford.org/articles/post-acute-withdrawal-syndrome
[32] - https://americanaddictioncenters.org/withdrawal-timelines-treatments/post-acute-withdrawal-syndrome
[33] - https://www.addictions.com/blog/building-a-healthy-support-system-in-recovery/
[34] - https://englishmountain.com/blog/building-support-system-recovery/
[35] - https://www.ncbi.nlm.nih.gov/books/NBK551500/
24/7 HELP
Begin your healing at Restore.
Restore Detox Centers is your 24-hour residential treatment facility for alcohol and drug addiction. Our compassionate team of professionals understands your challenges, providing effective rehabilitation services in San Diego. From medically assisted detox to comprehensive residential programs, we guide you towards a life free from addiction.
Stay connected with news and updates!
Join our mailing list to receive the latest news and updates from our team.
Don't worry, your information will not be shared.
We hate SPAM. We will never sell your information, for any reason.